COLON CANCER PREVENTION PROGRAM
COLORECTAL CANCER SCREENING
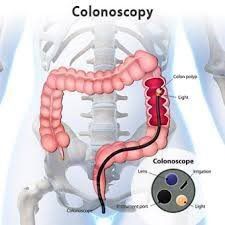
Colorectal cancer (CRC), often referred to as colon cancer, develops in the colon or the rectum (known as the large bowel or large intestine). The colon and rectum are parts of the digestive system, which is also called the gastrointestinal (GI) tract. The digestive system processes food for energy and eliminates solid waste. CRC usually develops slowly over many years. Most colorectal cancer begins as a noncancerous (benign) adenoma or polyp (abnormal growth) that develops on the lining of the colon or rectum. Polyps can be removed to significantly reduce cancer risk. Colonoscopy plays an important role in colorectal cancer prevention because precancerous polyps can be detected and removed during the same exam when they are discovered
Colorectal cancer is the second leading cause of cancer-related deaths in the United States (when men and women are combined). It is the third leading cause of cancer-related deaths when men and women are considered separately (behind lung and prostate cancer in men, and behind lung and breast cancer in women).
Nearly 137,000 people in the United States are diagnosed with colorectal cancer each year and over 50,000 die because of it annually.
The majority of CRC can be prevented with proper screening, early detection and removal of adenomatous polyps (precancerous polyps). Screening helps prevent CRC by finding precancerous polyps so they can be removed before they turn into cancer.
According to a 2013 report from the Centers of Disease Control and Prevention (CDC), about one in three adults (23 million) between the ages of 50 and 75 years old are not getting screened for colorectal cancer as recommended. Exercise and eating healthy foods such as vegetables and fruits can help decrease the risk of colorectal cancer, but screening is an essential part of colorectal cancer prevention.
As of November 2010, there is no federal law requiring all insurers to cover the cost of preventative CRC screenings. However, enactment of the Affordable Care Act requires coverage of CRC screenings for certain populations depending on an individual's insurance plan. So far only 30 states have passed laws requiring coverage for screening of CRC, a cancer causing 50,000 deaths per year. In contrast, 50 states have passed legislation requiring coverage of screening for breast cancer, a cancer causing 40,000 deaths per year. Additional efforts to improve colorectal cancer screening are needed. Medicare covers colonoscopy once every ten years for those 65 and over at average risk.
In February 2013, the federal government issued an important clarification on preventive screening benefits under the Affordable Care Act. Patients with private insurance will no longer be liable for cost sharing when a precancerous colon polyp is removed during screening colonoscopy. This ensures that colorectal cancer screening is available to privately insured patients at no additional cost, as intended by the new healthcare law. Patients with Medicare coverage must still pay a coinsurance when a polyp is removed as a result of the screening colonoscopy. Click here for the guidance language provided by the administration. Patients with private insurance should check with their individual providers to learn the details of their coverage and ask about the Affordable Care Act.
The incidence of CRC and the death rate from the disease has dropped for the past 15 years. Scientists believe that the decrease is probably because polyps are being found and removed by colonoscopy before becoming cancer. Also, CRC is being found earlier when it is easier to cure, and treatments for cancer once it has occurred have improved. There are approximately one million CRC survivors in the United States and that number is growing. According to American Cancer Society data released in 2014, colorectal cancer incidence rates have dropped 30 percent in the U.S. in the last 10 years among adults 50 and older due to the widespread uptake of colonoscopy.
The five-year survival rate for people with CRC discovered early is greater than 90 percent. But only 39 percent of CRCs are found at that early stage. Five-year survival rapidly declines when the cancer has spread to nearby organs or lymph nodes.
Individuals who have a family member (parent, brother or sister, or child) with colorectal cancer or polyps are at increased risk for developing the disease themselves and may need to undergo more aggressive screening starting at a younger age. Individuals who have more than one family member with colorectal cancer or with other types of cancers may be at even higher risk.
Symptoms of CRC
Certain symptoms might indicate this cancer:
Blood in the stool
Narrower than normal stools
Unexplained abdominal pain
Unexplained change in bowel habits
Unexplained anemia
If you experience any of these symptoms, talk with your physician. Crc can also occur without symptoms, family history, or any predisposing conditions such as inflammatory bowel disease. When a patient is being evaluated for symptoms, this is not considered screening but diagnostic evaluation. The term screening is reserved for healthy, asymptomatic patients.
Screening Recommendations For Those At Average Risk:
Beginning at age 50, both men and women at average risk for developing CRC should have a colonoscopy every 10 years. The risk of developing CRC increases with age, with more than 90 percent of cases occurring in persons aged 50 or older.
Men and women should begin screening earlier and more often if they have any of the following CRC risk factors: a family history of CRC or polyps, a known family history of inherited CRC syndromes, a personal history of CRC, or a personal history of chronic inflammatory bowel disease (ulcerative colitis or Crohn's Disease).
People with risk factors for CRC or family history of CRC should talk with a gastroenterologist about screening at an earlier age and find out how often they need to be screened. Read the Screening and Surveillance for the Early Detection of Colorectal Cancer and Adenomatous Polyps, 2008: A Joint Guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Endorsed by ASGE as part of the US Multi-Society Task Force on Colorectal Cancer.
There are several screening methods which have different abilities to detect or prevent CRC: stool blood test known as Fecal Occult Blood Test (FOBT) or Fecal Immunochemical Test (FIT), flexible sigmoidoscopy, colonoscopy, CT colonography, barium enema with air contrast, and stool DNA testing. Tests which mainly detect cancer include FOBT, FIT, and stool DNA. Tests which mainly detect polyps or cancer include colonoscopy, flexible sigmoidoscopy, CT colonography, barium enema, and colon capsule endoscopy. Colonoscopy is considered the gold standard of colorectal cancer screening methods for its ability to view the entire colon and both detect and remove polyps during the same procedure.
Patients should speak with their physician about the screening method that is best for them. To learn more about CRC prevention and available screening options, log on to ASGE's colorectal cancer awareness Web site www.screen4coloncancer.org.
Diet And Lifestyle:
There are no foods that directly cause colorectal cancer. However, studies of different populations have identified associations that may affect your risk of developing colorectal cancer. Smoking clearly increases the risk of colorectal cancer and other cancers. Studies have shown a slight increased risk of developing colorectal cancer among individuals with higher red meat or non-dairy (meat-associated) fat intake. Studies have also shown that getting an adequate amount of calcium and vitamin D in the diet or from supplements can reduce the risk of polyps and cancer. Use of aspirin and NSAIDs (such as celecoxib and sulindac) has been proven to decrease the risk of colorectal polyps. There may be a decreased risk of colorectal cancer in patients taking aspirin. However, the use of these agents is reserved for individuals at high risk for colorectal polyps and cancer.
Ongoing studies evaluating the role of vitamins and other natural products are underway to examine their role in colorectal cancer prevention. Few studies, though, have been able to show that modifying lifestyle reduces the risk of colorectal polyps or cancer. Nonetheless, lifestyle modifications such as reducing dietary fat, increasing fruits and vegetables, ensuring adequate vitamin and micro-nutrient intake, and exercise, may improve general health.
Regardless of your dietary and lifestyle habits, screening for colorectal polyps is the key in preventing colorectal cancer.
What African-Americans Should Know About CRC:
Although all men and women are at risk for CRC, some people are at higher risk for the disease because of age, lifestyle or personal and family medical history. According to studies, African-Americans are at a higher risk for the disease than other populations. Starting at age 50, everyone should begin routine screening tests. Research shows that African-Americans are being diagnosed at a younger average age than other people. Therefore, some experts suggest that African-Americans should begin their screening at age 45.
The incidence of CRC is higher among African-Americans than any other population group in the United States.
Death rates from CRC are higher among African-Americans than any other population group in the United States.
There is evidence that African-Americans are less likely than Caucasians to get screening tests for CRC.
African-Americans are less likely than Caucasians to have colorectal polyps detected at a time when they can easily be removed.
African-Americans are more likely to be diagnosed with CRC in advanced stages when there are fewer treatment options available. They are less likely to live five or more years after being diagnosed with CRC than other populations.
There may be genetic factors that contribute to the higher incidence of CRC among some African-Americans.
African-American women have the same chance of getting CRC as men, and are more likely to die of CRC than are women of any other ethnic or racial group.
African-American patients are more likely to have polyps deeper in the colon (on the right side of the colon).
What Hispanics Should Know About CRC:
Hispanic Americans are less likely to get screened for the disease than either Caucasians or African-Americans. Starting at age 50, everyone should begin routine screening tests.